Carney Hospital walks financial tightrope to avoid closing
Trims staff but plans to add addiction treatment center

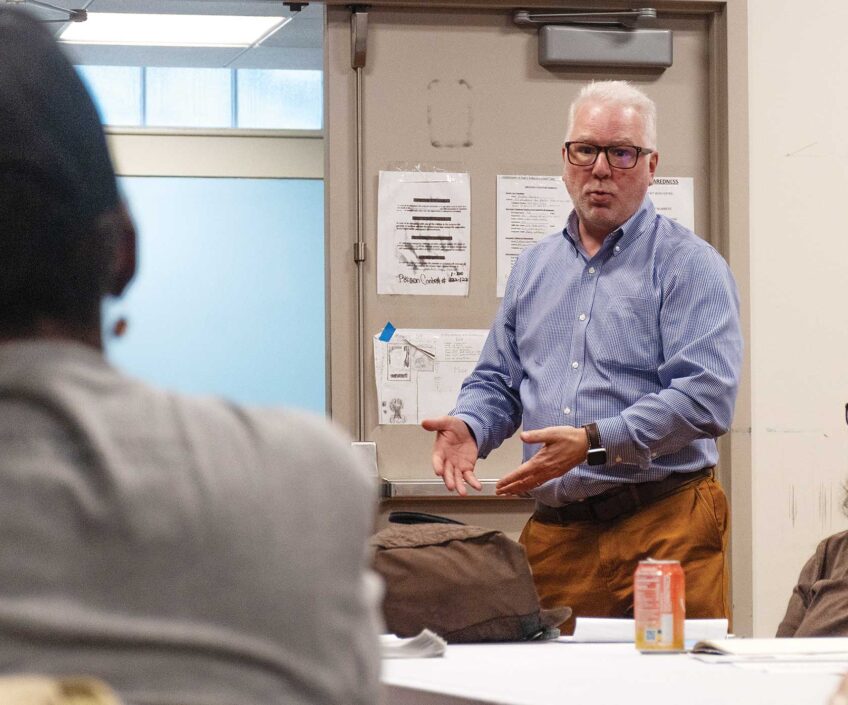
“I did not come here for the hospital to close,” said Stan McLaren, who in 2021 became CEO of Carney Hospital in Dorchester. “I haven’t heard anything from corporate about plans to close Carney.”
McLaren was referring to Carney’s owner, Steward Health Care.
Concerns about the hospital’s future surfaced when its four-year union contract with Carney nurses expired in December. Steward initially proposed a new contract of only one year.
“They’re worried about money, and they were saying they didn’t know what the future holds,” said Dana Simon, a director at the Massachusetts Nurses Union and part of the union’s bargaining team at Carney.
Fears of Carney’s demise aren’t eased by Steward’s actions in other states. It is closing one of its hospitals and has threatened to close another. Like Carney, they were financially struggling hospitals providing health care to underserved communities.
For most of its existence, Carney has operated as a nonprofit hospital. When Andrew Carney established the hospital in 1893, he said its mission was to care for all, regardless of who they were.
“We’re still committed to that,” McLaren said.
But Carney became a for-profit hospital after Steward Health Care bought it in 2010. Boston-based Steward grew to be the largest hospital network in New England, acquiring hospitals in other states and moving its headquarters to Texas in 2017.
Under Steward, Carney has gained, among other things, a 3-D mammography machine, an audiology booth for hearing tests, guest surgeons for outpatient surgeries, a wound care center for diabetic patients, new operating rooms, an emergency department facelift and a dialysis room for kidney patients.
But Carney has nearly always operated at a loss, McLaren said.
One reason is that most of its patients — up to 80% — use government-sponsored health insurance, such as MassHealth. It pays the hospital less for medical procedures and services than other insurers do. In addition, private insurers pay Carney less than other local hospitals for the same services.
“That just widens the gap with health disparities,” said Marisela Marrero, Steward’s health care equity and diversity director. “There’s no reason Carney’s payments should be so much less.”
In addition, there aren’t enough patients coming into Carney.
“People have forgotten what we have to offer,” said chief nursing officer Kellie Gouveia. “We have a state-of-the-art operating room and physical therapy and other services.”
“We are underutilized,” agreed McLaren. “We can take on more.”
The former president and CEO of Harvard Street Neighborhood Health Center pointed out that many hospitals are still recovering from the pandemic, when many people avoided hospitals and delayed routine medical care, such as mammograms and physicals. But he admits that outreach has become harder since Steward eliminated Carney’s public relations department a year ago.
“But I think Steward is aware of that,” he said.
Simon from the nurses’ union said that more patients would require more staff. He said that Steward has cut staff through layoffs and buyouts.
“Carney has to cap the number of patients they admit based on lack of staff,” Simon said. “When someone comes to the emergency room, they just stabilize the patient and send them somewhere else. Carney doesn’t have enough staff to admit them.”
In 2016, Steward sold its Boston-area hospital buildings to Medical Properties Trust (MPT), which then mortgaged them and leased them back to Steward. Now MPT holds the mortgage on the Carney Hospital building, the hospital is a tenant of MPT, and Steward pays the rent.
This is a typical arrangement, said Eileen Appelbaum, a health care economist and co-director of the Center for Economic and Policy Research in Washington, DC.
“MPT is a real estate investment trust, which requires its properties to make money for its investors,” she said, adding that companies like Steward increase profits by selling a hospital’s real estate, selling off part or all of a hospital’s services, cutting staff or limiting services.
Steward has its own financial troubles, according to news reports. Lawsuit settlements are one thing eating into its funds. They include a $4.7 million settlement with federal and Massachusetts governments for violating the False Claims Act. The company is also facing a class action lawsuit over medical privacy and social media.
According to Bloomberg, Steward has incurred billions of dollars in losses, and even requested an extension on multimillion-dollar loans from the federal government and others. MPT is also a small part-owner of Steward. As such, it has loaned funds to Steward for investments in its hospitals. Specific details are difficult to come by, as Steward prefers not to provide financial information, and has even sued the state for asking for it.
Meanwhile, the Massachusetts Center for Health Information and Analysis rated Steward’s financial solvency lower than that of any other hospital system in the state.
Other lawsuits come from creditors who claim Steward never paid them. Steward has countersued some creditors, claiming fraud or failure to provide promised products or services.
In May, Steward announced it was closing a hospital in San Antonio. Steward had taken over the Texas Vista Medical Center in 2017. The announced shutdown came after Steward failed to convince the county government or a university medical center to take it over.
Easton Hospital in the Pennsylvania city of the same name narrowly missed closing. The 133-year-old hospital was a nonprofit community medical center before Steward bought it in 2017. By March 2020, Steward was in talks with a potential buyer for the hospital. But even as the pandemic got underway, Steward threatened to close Easton unless it got a bailout.
In a March 22, 2020 letter, Steward stated, “If the Commonwealth has no interest in assuming all operating expenses and liabilities of Easton Hospital, Steward Health Care will proceed immediately on planning to close the facility.”
Appelbaum, the health economist, said Steward’s letter came just as federal pandemic stimulus funds were earmarked for struggling hospitals.
“Steward just wanted that pandemic money,” she said. “It was straight up blackmail.”
It worked. Days later, Pennsylvania guaranteed Steward $8 million immediately, with a likely $24 million to come later. Pennsylvania’s governor at the time, Tom Wolf, said most of the money would come from the federal pandemic stimulus funding.
Steward sold Easton Hospital four months later.
Closer to home, Steward closed Quincy Medical Center in 2014. Steward later sold the property and, in 2021, developers tore down the 124-year-old hospital, replacing it with a 465-unit apartment building.
Despite its problems, Steward has made some promising moves for Carney. During the pandemic, it served as the country’s only dedicated treatment hospital for COVID-19. In addition, plans are under way for a new outpatient addiction clinic McLaren is hoping will open by 2025. Meanwhile, Steward is closing the inpatient addiction center at its Taunton hospital.
The centrally located Carney may also absorb patients from Quincy-based Compass Medical Group. It suddenly closed its health centers in May after Steward successfully sued the company. Steward has reached out to Compass’ former patients on its website.
“We are steadfastly committed to ensuring Carney Hospital has the resources necessary to continue providing patient-centered, quality care to the community,” said Mark Girard, president of Steward, in an email in response to the Banner’s questions.
McLaren too remains optimistic.
“I don’t think Steward would invest this much in a hospital it intends to close,” he said.